Effectiveness of cognitive behavioral therapy-based interventions on health outcomes in patients with coronary heart disease: A meta-analysis
- ️Jing Sun
- ️Fri Nov 19 2021
Meta-Analysis Open Access
Copyright ©The Author(s) 2021. Published by Baishideng Publishing Group Inc. All rights reserved.
World J Psychiatr. Nov 19, 2021; 11(11): 1147-1166
Published online Nov 19, 2021. doi: 10.5498/wjp.v11.i11.1147
Effectiveness of cognitive behavioral therapy-based interventions on health outcomes in patients with coronary heart disease: A meta-analysis
Yan-Ni Li, Jing Sun, School of Medicine and Dentistry, Griffith University, Gold Coast Q4222, Queensland, Australia
Nicholas Buys, Jing Sun, Menzies Health Institute Queensland, Griffith University, Gold Coast Q4222, Queensland, Australia
Zhan-Jiang Li, The National Clinical Research Center for Mental Disorders and Beijing Key Laboratory of Mental Disorders, Beijing Anding Hospital, Beijing 100088, China
Zhan-Jiang Li, Advanced Innovation Center for Human Brain Protection, Capital Medical University, Beijing 100069, China
Author contributions: Sun J contributed to the paper conceptualization and design; Sun J and Li YN contributed to research design; Sun J and Li YN compiled studies and extracted data; Li YN conducted statistical and meta-analysis, completed table and figure presentation; Sun J and Li YN conducted writing of the paper; Buys N, Ferguson S and Li ZJ edited the draft; Sun J and Li YN revised and proofed the final revised version of the paper.
Conflict-of-interest statement: All authors declare no conflict of interests.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Corresponding author: Jing Sun, PhD, Associate Professor, School of Medicine and Dentistry, Griffith University, G40 8.23, Gold Coast Q4222, Queensland, Australia. j.sun@griffith.edu.au
Received: April 9, 2021
Peer-review started: April 9, 2021
First decision: July 14, 2021
Revised: July 27, 2021
Accepted: October 18, 2021
Article in press: October 18, 2021
Published online: November 19, 2021
Processing time: 221 Days and 20.4 Hours
Abstract
BACKGROUND
Recently, the efficacy of cognitive behavioral therapy (CBT)-based intervention on health outcomes in patients with coronary heart disease (CHD) has been recognized in randomized controlled trials (RCTs), but no comprehensive systematic review has been conducted. To address this research gap, our study aimed to evaluate whether comprehensive CBT-based interventions positively affect health outcomes in CHD patients. It was hypothesized that CBT-based interventions are effective in: (1) Reducing depression, anxiety, and stress symptoms; (2) Reducing body mass index, blood pressure, and lipid levels; and (3) Improving quality of life, and exercise endurance.
AIM
To verify the effectiveness of CBT-based interventions on CHD patients through a meta-analysis of previous publications.
METHODS
Relevant RCTs published in English were obtained by searching electronic databases, including PubMed, Embase, Cochrane Central Register of Controlled Trials, Scopus, and Proquest, with the retrieval time from inception to August 2020. The primary outcomes were psychological factors (depression, anxiety, and stress symptoms), physiological factors (body mass index, blood pressure, blood lipids). The secondary outcomes included quality of life and exercise endurance. We used Review Manager 5.3 to conduct the meta-analysis and used the Physiotherapy Evidence Database tool to evaluate the quality of studies.
RESULTS
A total of 22 RCTs comprising 4991 patients with CHD were included in the systematic review and meta-analysis. The main analysis revealed that CBT-based intervention can reduce depression symptoms: -2.00 [95% confidence interval (CI): -2.83 to -1.16, P < 0.001]; anxiety symptoms: -2.07 (95%CI: -3.39 to -0.75, P = 0.002); stress symptoms: -3.33 (95%CI: -4.23 to -2.44, P < 0.001); body mass index: -0.47 (95%CI: -0.81 to -0.13, P = 0.006); and improve physical functioning: 3.36 (95%CI: 1.63 to 5.10, P = 0.000) and mental functioning: 6.91 (95%CI: 4.10 to 9.73, P < 0.001). Moreover, subgroup analysis results showed that CBT-based interventions were more effective for symptoms of depression and anxiety in CHD patients when individual, as opposed to group treatment, and psycho-education, behavioral and cognitive strategies were applied as the core treatment approaches.
CONCLUSION
CBT-based interventions are effective treatment strategies for CHD patients, significantly improving their symptoms of depression, anxiety and stress, body mass index, and health-related quality of life.
Core Tip: This is the first comprehensive meta-analysis examining the effects of critical components of cognitive behavioral therapy (CBT) on improving health outcomes in coronary heart disease (CHD) patients. Our findings suggest that CBT-based interventions were effective in reducing depression, anxiety, stress symptoms, and body mass index levels, and improving physical and mental functioning of the quality of life. In addition, the intervention was more effective when it was delivered as an individual-based treatment, when there was no CHD-specific manual, and when psycho-education, behavioral, and cognitive strategies were applied as the key components of the CBT approach.
- Citation: Li YN, Buys N, Ferguson S, Li ZJ, Sun J. Effectiveness of cognitive behavioral therapy-based interventions on health outcomes in patients with coronary heart disease: A meta-analysis. World J Psychiatr 2021; 11(11): 1147-1166
- URL: https://www.wjgnet.com/2220-3206/full/v11/i11/1147.htm
- DOI: https://dx.doi.org/10.5498/wjp.v11.i11.1147
INTRODUCTION
Coronary heart disease (CHD), also known as ischemic heart disease, refers to arterial blockage and functional changes of the coronary artery, which then causes myocardial ischemia and hypoxia[1]. CHD patients are prone to have severe physical and mental problems and show the impaired health-related quality of life (QOL)[2], related to high mortality and additional cardiac events[3]. It has been reported that 7.4 million deaths worldwide were due to CHD[4]. Body mass index (BMI), blood pressure, total cholesterol (TC), low-density lipoprotein cholesterol, and glycosylated hemoglobin are important physiological factors observed in patients with CHD[5].
An increasing number of studies have shown that CHD is comorbid with the psychosomatic disease, and mental health plays a significant role in the development and progression of atherosclerosis and heart disease[6]. Doering et al[7] undertook a longitudinal cohort study with 2325 patients with stable CHD and found that depression and anxiety symptoms increased the risk of death in participants. Pająk et al[8] found a high prevalence of depression and anxiety in CHD patients, and that these psychological factors were negatively associated with favorable lifestyle changes, which were not conducive to CHD rehabilitation. A review by Cohen et al[9] indicated that chronic anxiety and exposure to daily stressors harmed cardiovascular health. The aggressive treatment of depression and anxiety is imperative because of the association of these factors with decreased medication compliance[10], lifestyle change adherence, and an increased risk of mortality[11].
Cognitive behavioral therapy (CBT) has been increasingly used to modify cardiovascular risk factors in psychosocial intervention programs[12,13] and to reduce psychosocial risk factors, including depression, anxiety, and loneliness, in patients with heart disease[14]. In general, CBT is a psychological therapy based on the hypothesis that cognitive processes affect emotion and behavior. Therefore, changing non-adaptive thought patterns and beliefs will lead to positive behavioral changes[15]. However, the effects of CBT on improving health outcomes in CHD patients are inconsistent. For instance, a cardiac rehabilitation program[16] showed that CBT was associated with significant improvement in depressive symptoms and high-density lipoprotein cholesterol (HDL-C). Similarly, Magán et al[17] found that psychological outcomes in CHD patients were improved when a CBT approach was implemented. However, Turner et al[18] found no differences between CBT and control groups on change in depression or anxiety symptoms in cardiac patients. Additionally, in most meta-analyses conducted to date, there has been no detailed analysis of the critical components of CBT affecting patients with CHD.
To address the research gap, this study aimed to evaluate whether CBT-based interventions are effective in reducing depression, anxiety and stress symptoms, BMI, blood pressure, and lipids level, improving QOL, and exercise endurance in CHD patients.
MATERIALS AND METHODS
We conducted this meta-analysis following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. In addition, we registered the research protocol at the PROSPERO International Prospective Register of Systematic Reviews (Registration ID: CRD42020213587 PROSPERO 2020 website: https://www.crd.york.ac.uk/prospero/#recordDetails). We did not need to get Ethical Approval or Patient Consent for this study, because it was a systematic review and meta-analysis based on the previous publications.
Search strategy
The databases, including PubMed, Embase, Cochrane Central Register of Controlled Trials, Scopus, Proquest, were searched separately by two researchers. The keywords of "coronary heart disease" or "unstable angina" or "percutaneous coronary intervention" or "coronary artery bypass graft" or "acute coronary syndrome" or "myocardial infarction" and "cognitive behavioral therapy" were used to do the literature retrieval. We used the subject words + free words with Boolean operators AND/OR to search for target articles in abstracts, keywords, or titles, and the language was limited to English. In the search process, we modified the search terms appropriate for different search rules of various databases. The specific retrieval strategy was in the supplementary file. The reference lists of the publications were searched to find additional relevant articles. The retrieved time was restricted from its inception to August 2020. We used the Endnote X8 Software (Clarivate Analytics, PA, United States) to manage the collected literature. The literature search was conducted separately by two researchers. When there was a disagreement between the two researchers, a third researcher was invited to join in the discussion to resolve the disagreement.
Study selection
Inclusion criteria were developed using the PICOS approach: (1) P: The target population was adult patients aged 18 and above and with diagnosed CHD, regardless of disease stage and severity. Eligible patients included those with unstable angina, those who had undergone percutaneous coronary intervention or coronary artery bypass graft, and patients with the acute coronary syndrome or those who had suffered a myocardial infarction; (2) I: The principles of CBT had to be applied to the intervention, including both cognitive and behavioral techniques, such as recognition and diagnosis of automatic thinking, behavior experiment, behavior activation, cognitive restructuring, and emotional modulation. A separate CBT or CBT combined with other methods was acceptable. The delivery of intervention could be face-to-face or remote, and the intervention form could be individual or group-based; (3) C: The control groups could be the non-CBT interventions, or usual care or waiting list. The usual care group was chosen if there were multiple comparison groups; (4) O: The main outcomes were psychological factors, including depression, anxiety, and stress symptoms; physiological factors, including BMI, blood pressure, lipids level: Low-density lipoprotein cholesterol, HDL-C, triglycerides, TC. The secondary outcomes were QOL and exercise endurance. 6-Minute Walk Distance Test was used to assess the exercise endurance. The article reporting one or more of the above outcomes was included; (5) S: We included the randomized controlled trial (RCT), with no limitation on follow-up time; (6) Only English articles; and (7) Accessibility of full-text publication.
Studies were excluded based on the following criteria: (1) Comprising solely cognitive or behavioral therapies; (2) No report on quantitative analyses; (3) All reviews and protocols; (4) Literature with incomplete data and inconsistent statistical methods; (5) Duplicate publications, we only included the most relevant study; (6) Low-quality studies, whose score of Physiotherapy Evidence Database tool (PEDro) ≤ 3; (7) Not English articles; or (8) Not a peer-reviewed journal article.
Data extraction
We extracted data by using a data-collection form, which included the following information: The name of the first author, publication year, research location, research subjects (sample size, age, sex, the type of diseases), research design, intervention method, control method, and outcome factors. Where data was incomplete, the corresponding author was contacted to obtain the data.
Quality assessment
The full texts of included articles were read by two reviewers independently and PEDro tool[19] was used to evaluate their methodological quality. There were ten items in PEDro tool: Subjects were randomly grouped; randomization was concealed; the baseline information between groups was similar; subjects, researchers, and assessors were blinded; low drop-out rate; "intention to treat" principle was used; the variability measures were used; between-group comparison methods were used. The quality of studies is categorized into three levels based on the ten items of PEDro tool: Research with eight points and above is high quality, with four to seven is medium quality, with three and less than three is low quality. The disagreements on the quality rating of the included study were resolved through consultation with a third researcher.
Statistical analysis
Review Manager 5.3 was used for the meta-analysis. We did a separate meta-analysis for each outcome variable. We used the pooled mean difference (MD) with a 95% confidence interval (CI) for continuous outcome variables and used the standardized MD (SMD) with 95%CI to measure their effect size. The effect size was small if SMD was between 0.2 and 0.5. When SMD ranged from 0.5 to 0.7, the effect size was medium. And the effect size was large when SMD was more than 0.7. The threshold was set as 0.05 and two-sided.
We used the Chi-square test and I2 for heterogeneity testing. If I2 < 50% or P > 0.05, homogeneity was considered to be good among the included studies, and the fixed-effect model was adopted. If I2 > 50%, studies were assessed as having a high level of heterogeneity, and the random-effect model was adopted.
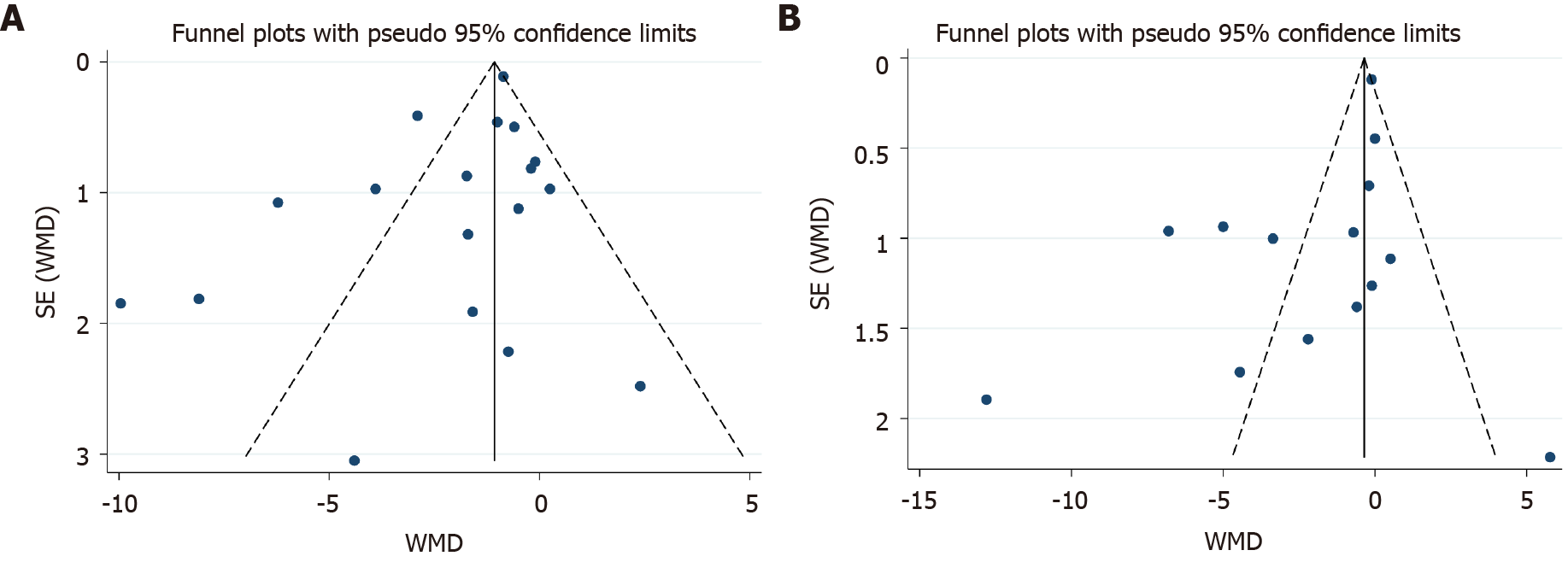
Publication bias was evaluated using the Egger test using Stata Statistical Software 15. There was a statistical publication bias if the P value was less than 0.05. In addition, we used the funnel plot to analyze whether there was publication bias if the number of meta-analysis studies exceeded 10.
Subgroup analyses were conducted for depression and anxiety symptoms in CHD patients to find the underlying factors that led to heterogeneity and to figure out the effective components of CBT. We evaluated the pooled MD for each subgroup and used the Q statistics to examine the differences in MD. The subgroups were as follow: The treatment form (individual or group); treatment course (< 12 wk or ≥ 12 wk); duration of a session (< 50 min or ≥ 50 min); the number of sessions (< 10 or ≥ 10); mode of delivery (face-to-face or remote); use of a CHD-specific manual (yes or no); drop-out rate (< 20% or ≥ 20%); the intervention group used specific techniques of CBT (yes or no). We categorized the specific techniques for CBT based on the Comprehensive Psycho-therapeutic Intervention Rating Scale and previous studies[20-23], which included psycho-education, behavioral strategies, cognitive strategies, affective strategies, interpersonal strategies, exposure, body-directed strategies, behavior experiment, mindfulness and attention, homework assignment. If the intervention technique was mentioned as an important technique, it was identified as "yes", otherwise it was identified as "no".
RESULTS
Literature search
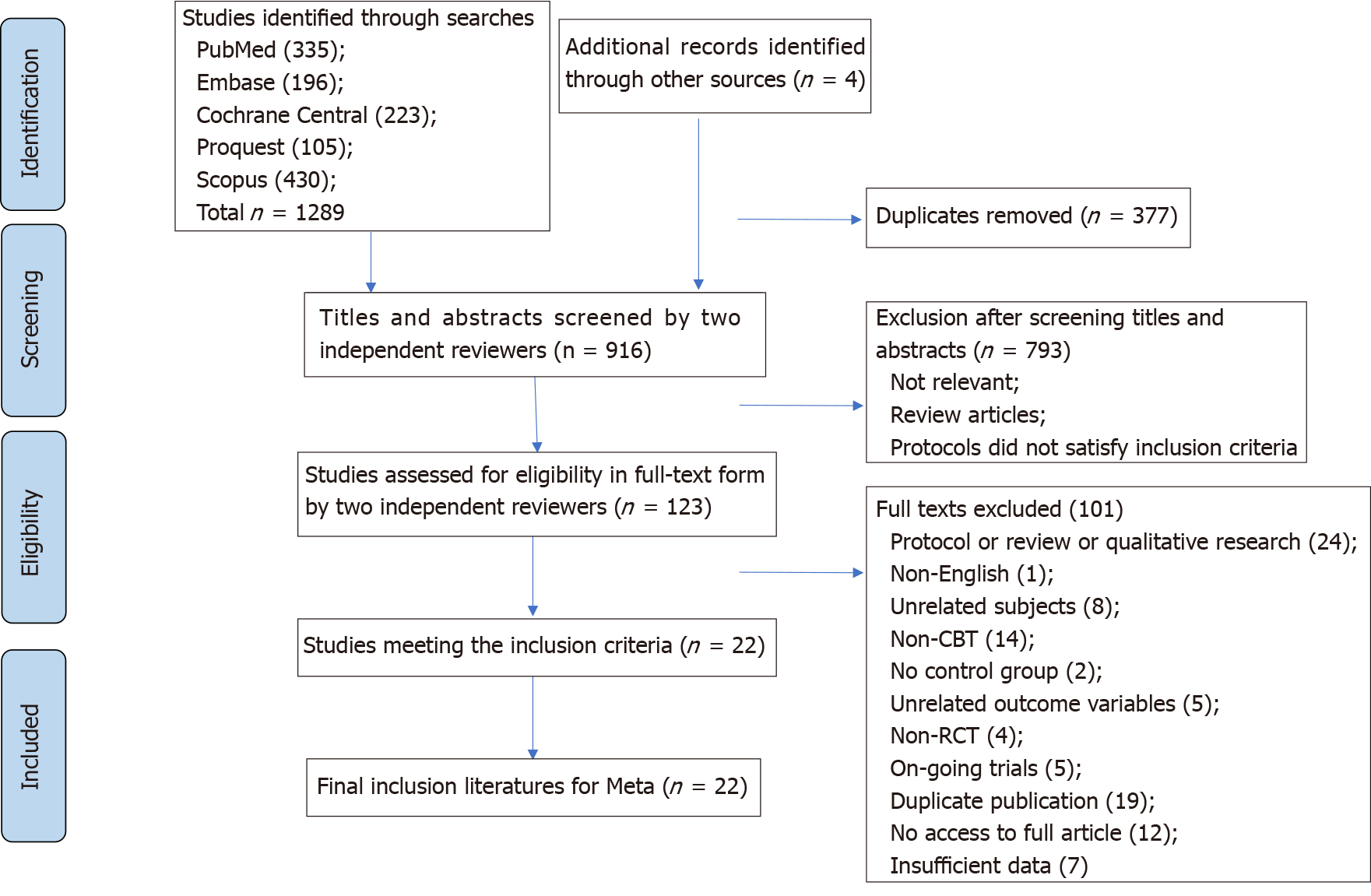
As shown in Figure 1, we found 1293 articles, including 1289 articles from the database search and four articles from references in the publications. After removing duplicates, there were 916 articles left for the title and abstract screening. Of these, we discarded 793 publications that did not meet the inclusion criteria. Then, 123 articles were left for the full-text screening. Two researchers independently did the full-text evaluation in strict accordance with the inclusion rules. Through full-text screening, 101 articles were excluded, and the specific process of identifying relevant articles for inclusion in the systematic review and meta-analysis was described in Figure 1, resulting in 22 studies being included in this meta-analysis.
Study characteristics
Full details of the included studies were displayed in Table 1. Four thousand nine hundred and ninety-one participants were included in the 22 RCTs: 2443 in the intervention group and 2548 in the control group. The mean age of the intervention group was 59.57 and 59.85 in the control group. Five[24-28] of these studies were carried out in developing countries and 17[14,16,18,29-42] in developed countries. The intervention group used CBT or CBT-based intervention and the control group adopted usual care methods activity methods. Five studies[34,38-41] used remote interventions, such as through the internet or telephone, and 17[14,16,18,24-33,35-37,42] used traditional face-to-face interventions. Twelve[16,24-26,29,32-34,38-40,42] studies used an individual CBT intervention, eight studies[18,27,30,31,35-37,41] used a group-based CBT intervention, and one[14] used both. Only six studies[18,24,29,33,37,41] reported using an instruction manual. Five types of outcomes were included in the analysis: physiological factors, psychological factors, QOL, exercise endurance, and cardiac rehabilitation factors. Six studies[16,31,34,37,41,42] reported physiological factors, 20 studies[14,16,18,25-36,38-42] reported psychological factors, 10[24,25,30-34,39,40,42] reported QOL, two[37,41] reported exercise endurance, and four[16,24,31,37] reported cardiac rehabilitation factors. However, due to the differences in cardiac rehabilitation factors, a meta-analysis could not be performed. The mean drop-out rate for the intervention group was 12.49% and 11.09% for the control group. Table 1 showed the characteristics of intervention methods and control methods in detail.
Table 1 Characteristics of randomized controlled trials included in this meta-analysis.
| Ref. | Country | Sample size (I/C) | Gender: female, n (%) | Age (mean ± SD) | CHD diagnosis | Intervention | Format | Manual | Control group | Outcome | Measurement | Drop-out rate (%) | Quality of article |
| Barth et al[29], 2005 | Germany | 59 (27/32) | I: 5 (18.50) C: 9 (28.10) | I: 60.81 ± 11.06 C: 55.62 ± 10.05 | MI; CABG; PTCA; Unstable Angina Pectoris | CBT based intervention | Individual | Yes | UC | (2) | BDI; HADS | I: 0.00 C: 12.50 | 7 (moderate) |
| Beresnevaitė et al[24], 2016 | Lithuania | 150 (79/71) | I: 13 (30.20) C: 14 (30.40) | I: 56.70 ± 10.20 C: 59.10 ± 11.10 | CABG; valve replacement; valve repair surgery | CBT | Individual | Yes | UC | (3), (5) | SF36 | I: 45.57 C: 35.21 | 4 (moderate) |
| Berkman et al[14], 2003 | United States | 2481 (1238/1243) | I: 532 (43.00) C: 552 (44.00) | I: 61.00 ± 12.60 C: 61.00 ± 12.50 | MI | CBT | Individual + group | No | UC | (2) | BDI | I: 7.51 C: NR | 7 (moderate) |
| Blumenthal et al[30], 2016 | United States | 151 (76/75) | I: 31 (41.00) C: 24 (32.00) | I: 61.80 ± 10.80 C: 60.40 ± 10.60 | ACS; stable angina; coronary revascularization | CR + SMT | Group | No | CR | (2), (3) | BDI-II; STAI; PSS; GHQ | I: 3.95 C: 4.00 | 7 (moderate) |
| Claesson et al[31], 2006 | Sweden | 198 (101/97) | I: 101 (100.00) C: 97 (100.00) | I: 59.40 ± 9.30 C: 62.20 ± 7.70 | AMI; CABG; coronary angioplasty; angina pectoris | CBT based intervention | Group | No | UC | (1), (2), (3), (5) | ELSS; CPRS-S-A | I: 23.76 C: 15.46 | 6 (moderate) |
| Dao et al[32], 2011 | United States | 100 (50/50) | I: 11 (22.90) C: 10 (20.40) | I: 62.80 ± 11.80 C: 64.20 ± 11.90 | A CAD diagnosis and were scheduled to undergo a first-time CABG | CBT | Individual | No | UC | (2), (3) | BDI-II; STAI SF12 | I: 4.00 C: 4.00 | 6 (moderate) |
| Freedland et al[33], 2009 | United States | 123 (41/42/40)1 | I: 23 (56.00) C1: 21 (50.00) C2: 17 (43.00) | I: 62.00 ± 11.00 C1: 59.00 ± 10.00 C2: 61.00 ± 9.00 | CABG | CBT + UC | Individual | Yes | SSM+ UC; UC | (2), (3) | BDI; BAI PSS; SF36 | I: 2.44 C1: 11.90 C2: 7.50 | 7 (moderate) |
| Javaheri et al[34], 2020 | United States | 34 (18/16) | I: 7 (38.89) C: 2 (12.50) | I: 70.30 ± 10.00 C: 72.90 ± 9.20 | MI; coronary artery revascularization; angiographically documented stenosis of a major coronary artery | General sleep education + web-based CBT | Individual | No | Wait-list | (1), (2), (3) | PHQ-8; Duke Health Profile | I: 16.67 C: 11.11 | 5 (moderate) |
| Koertge et al[38], 2008 | Sweden | 247 (119/128) | I: 119 (100.00) C: 128 (100.00) | I: 61.36 ± 9.10 C: 62.73 ± 8.72 | AMI; PCI; CABG | CBT based intervention | Group | No | UC | (2) | BDI | I: 17.65 C: 20.31 | 7 (moderate) |
| Lv et al[25], 2016 | China | 75 (38/37) | I: 12 (31.58) C: 10 (27.03) | I: 52.40 ± 6.30 C: 52.00 ± 6.20 | PCI | CBT + UC | Individual | No | UC | (2), (3) | HAM-D HAM-A CROQ-PTCA-POST | I: 0.00 C: 0.00 | 6 (moderate) |
| Merswolken et al[36], 2011 | Germany | 62 (30/32) | I: 6 (24.00) C: l8 (30.00) | I: 62.50 ± 8.30 C: 59.80 ± 7.50 | MI; angiographically documented CHD | CBT based intervention | Group | No | Blank control | (2) | HADS | I: 16.67 C:15.63 | 5(moderate) |
| Murphy et al[37], 2013 | Australia | 275 (139/136) | I: 15 (10.79) C: 22 (16.18) | I: 58.02 ± 8.87 C: 59.92 ± 9.27 | MI; CABG; PCI | CBT | Group | Yes | UC | (1), (4), (5) | 6MWT | I: 14.39 C: 16.91 | 7 (moderate) |
| Nehra et al[26], 2012 | India | 50 (25/25) | NR | NR | MI; AP | CBT | Individual | No | UC | (2) | PSS | I: 0.00 C: 0.00 | 5 (moderate) |
| Nejati et al[27], 2020 | Iran | 51 (17/17/17)2 | I: 7 (41.18) C1: 4 (23.53) C2: 5 (29.41) | I: 59.00 ± 10.48 C1: 57.00 ± 9.17 C2: 58.00 ± 9.77 | CABG; coronary angiography | CBTG | Group | No | CTG; UC | (2) | BDI-II; DASS-21 | I: 0.00 C: 0.00 | 6 (moderate) |
| Norlund et al[38], 2018 | Sweden | 239 (117/122) | I: 44 (37.60) C: 36 (29.50) | I: 58.40 ± 9.00 C: 60.80 ± 7.80 | MI | iCBT | Individual | No | UC | (2) | HADS | I: 17.95 C: 5.74 | 7 (moderate) |
| O’Neil et al[39], 2014 | Australia | 121 (61/60) | I: 16 (26.20) C:14 (23.30) | I: 61.00 ± 10.20 C: 58.90 ± 10.70 | ACS; unstable angina | CBT based intervention(telephone) | Individual | No | UC | (2), (3) | PHQ-9;SF-12 | I: 13.11 C: 11.67 | 9 (high) |
| Rafanelli et al[16], 2020 | Italy | 100 (50/50) | I: 19 (38.00) C: 12 (24.00) | I: 57.64 ± 9.99 C: 60.02 ± 10.94 | MI; unstable angina | CBT + WBT | Individual | No | CM | (1), (2), (5) | SQ | I: 16.00 C: 20.00 | 7 (moderate) |
| Schneider et al[40], 2020 | Canada | 53 (25/28) | I: 12 (48.00) C: 19 (67.90) | I: 56.72 ± 11.90 C: 59.29 ± 6.93 | MI; unstable angina | iCBT | Individual | No | Wait-list | (2), (3) | PHQ-9;GAD-7; DASS-21;SF-12 | I: 12.00 C: 7.14 | 7 (moderate) |
| Turner et al[18], 2013 | Australia | 57 (25/32) | I: 6 (24.00) C: 5 (28.13) | I: 61.00 ± 11.00 C: 62.00 ± 9.00 | ACS; PCI; CABG | CBT | Group | Yes | BI | (2) | BDI-II;HADS-A | I: 16.00 C: 3.13 | 7 (moderate) |
| Turner et al[41], 2014 | Australia | 42 (21/21) | I: 3 (14.29) C: 6 (28.57) | I: 55.60 ± 8.80 C: 57.00 ± 11.20 | AMI; CABG; PCI | iCBT | Group | Yes | UC | (1), (2), (4) | BDI-II; HADS-A 6MWT | I: 28.57 C: 23.81 | 5 (moderate) |
| Zeighami et al[28], 2018 | Iran | 90 (30/30/30)3 | I: 10 (33.33) C1: 9 (29.90) C2: 12 (40.10) | 47.62 ± 8.93 | MI | CBT | Nr | No | EMDR | (2) | BAI | NR | 4 (moderate) |
| Zetta et al[42], 2011 | United Kingdom | 233 (116/117) | I: 31 (28.00) C: 38 (35.00) | I: 64.80 ± 10.04 C: 65.94 ± 9.96 | Angina | CBT based intervention | Individual | No | UC | (1), (2), (3) | HADS; SF-36 | I: 6.03 C: 6.84 | 7 (moderate) |
Post- to pre-treatment effects of CBT-based intervention
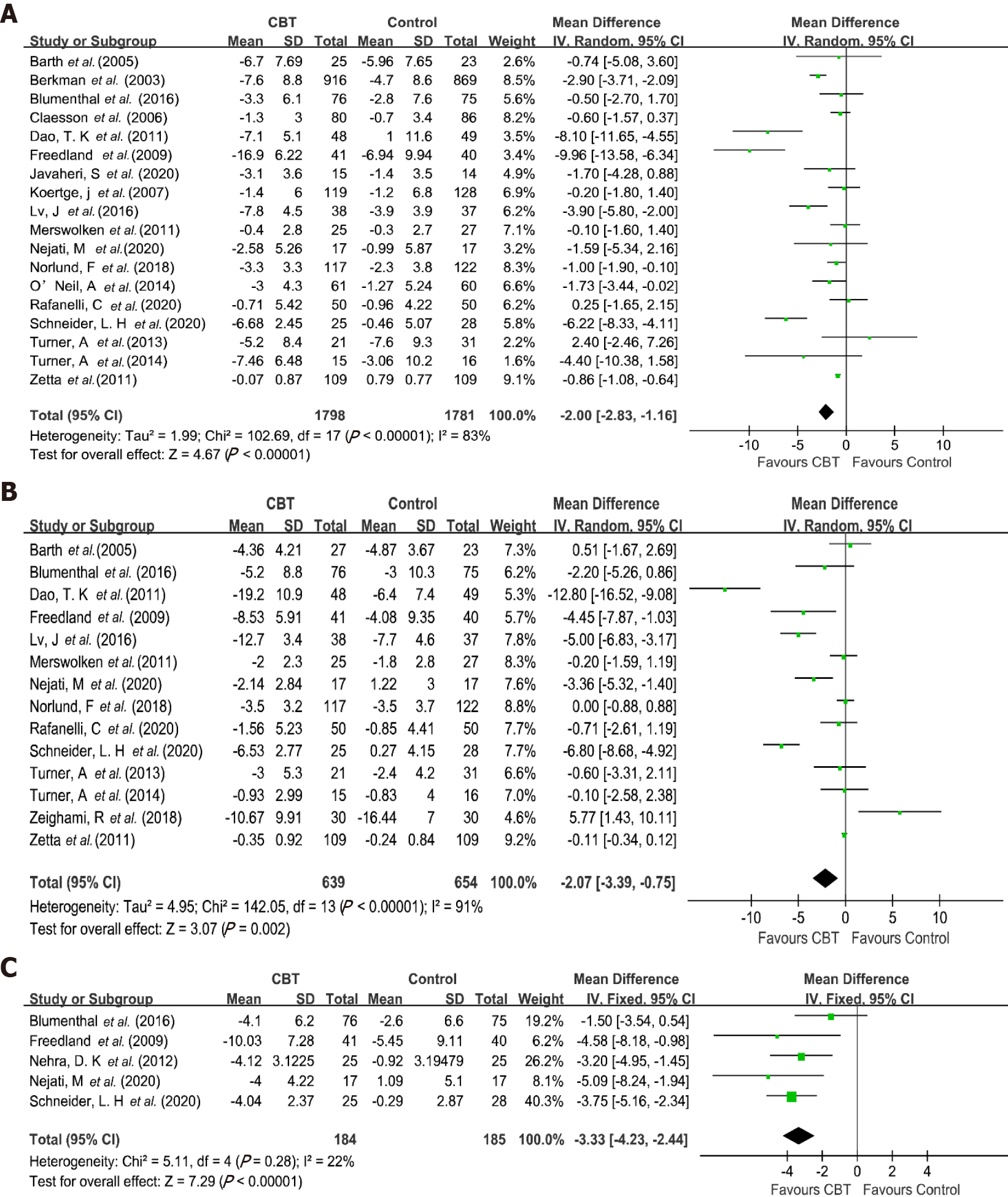
Effects on psychological factors: Eighteen studies[14,16,18,25,27,29-36,38-42] analyzed the effect of CBT-based intervention on depression symptoms in 3579 participants. The number of intervention and control group participants was 1798 and 1781, respectively. Results showed a significant improvement in depression symptoms, with a reduction of depression symptoms of -2.00 (95%CI: -2.83 to -1.16, P < 0.001), and a small effect size of SMD -0.42 (95%CI: -0.60 to -0.24, P < 0.001). There was statistical heterogeneity across the 18 studies (I2 = 83%, P < 0.001) (Table 2). The forest plot of the effect was shown in Figure 2A.
Figure 2 Forest plots of the effects of cognitive behavioral therapy-based interventions. A: Depression symptom; B: Anxiety symptom; C: Stress symptom. CBT: Cognitive behavioral therapy; CI: Confidence interval.
Table 2 Total effect of cognitive behavioral therapy -based interventions on depression, anxiety, stress symptoms, body mass index, blood pressure, total cholesterol, high-density lipoprotein cholesterol, quality of life, and 6-min walk test distance.
| Index | Outcomes: Post-to pre-treatment effect | |||||||
| Studies, n | Participant | I2 % (P value) | Q-test | MD (95%CI) | P value | SMD (95%CI) | P value | |
| Depression | 18 | 3579 | 83 (< 0.001) | 102.69 | -2.00 (-2.83, -1.16)c | < 0.001 | -0.42 (-0.60, -0.24)c | < 0.001 |
| Anxiety | 14 | 1293 | 91 (< 0.001) | 142.05 | -2.07 (-3.39, -0.75)b | 0.002 | -0.42 (-0.72, -0.11)b | 0.008 |
| Stress | 5 | 369 | 22 (0.280) | 5.11 | -3.33 (-4.23, -2.44)c | < 0.001 | -0.62 (-0.83, -0.40)c | < 0.001 |
| BMI | 2 | 377 | 0 (0.550) | 0.36 | -0.47 (-0.81, -0.13)b | 0.006 | -0.23 (-0.43, -0.02)a | 0.030 |
| Systolic pressure | 4 | 437 | 1 (0.390) | 3.04 | -1.82 (-5.12, 1.49) | 0.280 | -0.10 (-0.29, 0.09) | 0.290 |
| Diastolic pressure | 4 | 437 | 0 (0.870) | 0.72 | -0.95 (-2.75, 0.86) | 0.300 | -0.09 (-0.28, 0.09) | 0.330 |
| TC | 2 | 131 | 0 (0.390) | 0.75 | 0.15 (-0.81, 1.12) | 0.760 | 0.15 (-0.19, 0.50) | 0.380 |
| HDL-C | 2 | 131 | 0 (0.890) | 0.02 | 0.07 (-0.09, 0.23) | 0.390 | 0.05 (-0.29, 0.40) | 0.760 |
| Physical function | 7 | 666 | 49 (0.070) | 11.77 | 3.36 (1.63, 5.10)c | 0.000 | 0.27 (0.12, 0.43)b | 0.001 |
| Mental function | 5 | 419 | 52 (0.080) | 8.28 | 6.91 (4.10, 9.73)c | < 0.001 | 0.71 (0.41, 1.00)c | < 0.001 |
| 6-minute walk test distance | 2 | 279 | 0 (0.550) | 0.35 | 9.64 (-11.80, 31.08) | 0.380 | 0.11 (-0.13, 0.34) | 0.380 |
Subgroup analyses (Table 3) found that CBT-based intervention was more effective on improving depression symptoms when it was individual treatment form, when there was no CHD-specific manual, and when the drop-out rate was < 20%. CBT-based interventions statistically reduced depression symptoms when they emphasized psycho-education, behavioral and cognitive strategies as the core approaches. In addition, CBT-based intervention was more effective when it did not highlight affective or interpersonal strategies.
Table 3 Subgroup analysis on the effect of cognitive behavioral therapy-based interventions on depression symptoms.
| Subgroups | Depressive symptom: Post- to pre-treatment effect | ||||||
| Studies (n) | Participants (n) | I2 % (P value) | Q-test | MD (95%CI) | SMD (95%CI) | P value (between) | |
| Treatment form | 0.030 | ||||||
| Group | 8 | 2581 | 72 (0.001) | 24.86 | -0.96 (-2.16, 0.24) | -0.17 (-0.32, -0.02)a | |
| Individual | 10 | 1061 | 88 (< 0.001) | 75.51 | -2.97 (-4.33, -1.62)c | -0.66 (-0.97, -0.35)c | |
| Treatment course | 0.200 | ||||||
| ≥ 12 wk | 11 | 3194 | 81 (< 0.001) | 51.97 | -1.28 (-2.07, -0.50)b | -0.34 (-0.54, -0.14)c | |
| < 12 wk | 6 | 288 | 68 (0.008) | 15.69 | -2.83 (-5.08, -0.57)a | -0.54 (-1.05, -0.02)a | |
| Duration of a session | 0.070 | ||||||
| ≥ 50 min | 11 | 2788 | 84 (< 0.001) | 62.43 | -2.25 (-3.68, -0.81)b | -0.34 (-0.55, -0.13)b | |
| < 50 min | 3 | 439 | 13 (0.320) | 2.30 | -0.86 (-1.36, -0.35)c | -0.46 (-1.11, 0.19) | |
| Number of sessions | 0.330 | ||||||
| ≥ 10 | 9 | 2876 | 82 (< 0.001) | 43.75 | -1.62 (-2.76, -0.49)b | -0.28 (-0.45, -0.12)c | |
| < 10 | 8 | 485 | 80 (< 0.001) | 35.88 | -2.90 (-5.22, -0.59)a | -0.50 (-0.92, -0.09)b | |
| Treatment delivery way | 0.410 | ||||||
| Remote | 5 | 473 | 81 (0.000) | 20.63 | -2.73 (-4.78, -0.67)b | -0.58 (-0.97, -0.19)b | |
| Face to face | 13 | 3106 | 85 (< 0.001) | 77.45 | -1.77 (-2.78, -0.77)c | -0.37 (-0.59, -0.16)c | |
| Manual available | 0.610 | ||||||
| Yes | 4 | 212 | 84 (0.000) | 19.24 | -3.27 (-9.09, 2.55) | -0.39 (-1.07, 0.30) | |
| No | 14 | 3367 | 83 (< 0.001) | 76.32 | -1.76 (-2.56, -0.96)c | -0.42 (-0.62, -0.23)c | |
| Drop-out | 0.610 | ||||||
| ≥ 20% | 2 | 197 | 34 (0.220) | 1.51 | -1.31 (-4.21, 1.59) | -0.23 (-0.51, 0.05) | |
| < 20% | 16 | 3382 | 85 (< 0.001) | 100.58 | -2.10 (-3.04, -1.17)c | -0.44 (-0.64, -0.24)c | |
| Psycho-education strategies | 0.440 | ||||||
| Important | 15 | 3367 | 82 (< 0.001) | 76.48 | -1.78 (-2.59, -0.97)c | -0.40 (-0.59, -0.21)c | |
| Not important | 3 | 212 | 92 (< 0.001) | 24.52 | -4.60 (-11.79, 2.58) | -0.54 (-1.37, 0.28) | |
| Behavioral strategies | 0.005 | ||||||
| Important | 13 | 3315 | 87 (< 0.001) | 95.77 | -2.48 (-3.47, -1.48)c | -0.52 (-0.73, -0.31)c | |
| Not important | 5 | 264 | 11 (0.340) | 4.50 | -0.30 (-1.45, 0.85) | -0.05 (-0.30, 0.20) | |
| Cognitive strategies | 0.670 | ||||||
| Important | 16 | 3448 | 85 (< 0.001) | 99.64 | -2.11 (-2.99, -1.23)c | -0.45 (-0.64, -0.26)c | |
| Not important | 2 | 131 | 53 (0.150) | 2.11 | -1.18 (-5.38, 3.03) | -0.14 (-0.65, 0.37) | |
| Affective strategies | 0.005 | ||||||
| Important | 2 | 413 | 0 (0.680) | 0.18 | -0.49 (-1.32, 0.34) | -0.09 (-0.29, 0.10) | |
| Not important | 16 | 3166 | 85 (< 0.001) | 100.55 | -2.32 (-3.30, -1.33)c | -0.47 (-0.68, -0.27)c | |
| Interpersonal strategies | 0.230 | ||||||
| Important | 4 | 2422 | 80 (0.002) | 15.31 | -1.29 (-2.67, 0.09) | -0.21 (-0.37, -0.05)b | |
| Not important | 14 | 1157 | 84 (< 0.001) | 80.72 | -2.40 (-3.55, -1.25)c | -0.52 (-0.79, -0.24)c | |
| Body directed strategies | 0.070 | ||||||
| Important | 9 | 2876 | 70 (0.001) | 26.46 | -1.20 (-1.91, -0.49)c | -0.33 (-0.53, -0.12)b | |
| Not important | 9 | 703 | 88 (< 0.001) | 66.33 | -3.47 (-5.84, -1.10)b | -0.54 (-0.92, -0.17)b | |
| Homework assignment strategies | 0.890 | ||||||
| Important | 6 | 2314 | 83 (< 0.001) | 29.48 | -2.07 (-3.75, -0.38)b | -0.32 (-0.60, -0.05)a | |
| Not important | 12 | 1265 | 80 (< 0.001) | 55.64 | -1.93 (-2.96, -0.90)c | -0.47 (-0.74, -0.20)c |
The effect on anxiety symptoms was analyzed in 14 studies[16,18,25,27-30,32,33,36,38,40-42] with 1293 patients. There were 639 patients in the intervention group and 654 in the control group. The meta-analysis showed that CBT-based interventions significantly alleviated anxiety symptoms, with a reduction of symptom mean of -2.07 (95%CI: -3.39 to -0.75, P = 0.002), and a small effect size of -0.42 (95%CI: -0.72 to -0.11, P = 0.008). The heterogeneity was significant among the studies (I2 = 91%, P < 0.001) (Table 2). Figure 2B showed the forest plot of the effect.
Similarly, subgroup analyses (Table 4) found that CBT-based intervention was more effective for anxiety symptoms when it was individual treatment form, longer duration of a session (≥ 50 min), less than 10 sessions (< 10), face-to-face treatment delivery, and no use of CHD-specific manual. As for CBT technique components, CBT-based intervention was more effective when it applied the following techniques as the core strategies: psycho-education, behavioral and cognitive strategies. In addition, CBT-based interventions that did not use interpersonal strategy as the core approach showed a better effect on reducing anxiety symptoms.
Table 4 Subgroup analysis on the effect of cognitive behavioral therapy-based interventions on anxiety symptoms.
| Subgroups | Anxiety symptom: Post- to pre-treatment effect | ||||||
| Studies (n) | Participant (n) | I2 % (P value) | Q-test | MD (95%CI) | SMD (95%CI) | P value (between) | |
| Treatment form | 0.100 | ||||||
| Group | 5 | 320 | 50 (0.090) | 7.96 | -1.24 (-2.63, 0.15) | -0.27 (-0.57, 0.04) | |
| Individual | 8 | 913 | 94 (< 0.001) | 123.83 | -3.25 (-5.17, -1.32)b | -0.62 (-1.05, -0.18)b | |
| Treatment course | 0.280 | ||||||
| ≥ 12 wk | 8 | 935 | 73 (0.001) | 25.76 | -0.73 (-1.69, 0.23) | -0.16 (-0.40, 0.08) | |
| < 12 wk | 5 | 261 | 90 (< 0.001) | 38.38 | -2.47 (-5.48, 0.54) | -0.63 (-1.37, 0.12) | |
| Duration of session | 0.050 | ||||||
| ≥ 50 min | 9 | 652 | 89 (< 0.001) | 71.35 | -2.49 (-4.88, -0.09)a | -0.43 (-0.86, -0.00) | |
| < 50 min | 2 | 318 | 0 (0.540) | 0.38 | -0.12 (-0.35, 0.11) | -0.13 (-0.35, 0.09) | |
| Number of session | 0.150 | ||||||
| ≥ 10 | 6 | 617 | 79 (0.000) | 23.89 | -0.98 (-2.77, 0.80) | -0.18 (-0.54, 0.18) | |
| < 10 | 7 | 458 | 92 (< 0.001) | 70.66 | -3.50 (-6.42, -0.58)a | -0.66 (-1.23, -0.10)a | |
| Treatment delivery way | 0.390 | ||||||
| Remote | 4 | 383 | 94 (< 0.001) | 51.28 | -0.59 (-4.68, 3.51) | -0.29 (-1.17, 0.59) | |
| Face to face | 10 | 910 | 90 (< 0.001) | 88.49 | -2.54 (-4.17, -0.90)b | -0.47 (-0.78, -0.16)b | |
| Manual available | 0.200 | ||||||
| Yes | 4 | 214 | 50 (0.110) | 6.03 | -0.86 (-2.73, 1.02) | -0.19 (-0.52, 0.13) | |
| No | 10 | 1079 | 93 (< 0.001) | 135.85 | -2.48 (-4.12, -0.84)b | -0.52 (-0.91, -0.12)a | |
| Psycho-education strategies | 0.140 | ||||||
| Important | 10 | 1021 | 93 (< 0.001) | 128.71 | -2.71 (-4.29, -1.13)c | -0.57 (-0.95, -0.19)b | |
| Not important | 4 | 272 | 77 (0.004) | 13.30 | -0.14 (-3.14, 2.86) | -0.03 (-0.54, 0.48) | |
| Behavioral strategies | 0.003 | ||||||
| Important | 9 | 998 | 94 (< 0.001) | 134.13 | -3.46 (-5.33, -1.60)c | -0.67 (-1.07, -0.27)b | |
| Not important | 5 | 295 | 47 (0.110) | 7.57 | 0.13 (-1.27, 1.54) | 0.05 (-0.26, 0.36) | |
| Cognitive strategies | 0.020 | ||||||
| Important | 11 | 1102 | 93 (< 0.001) | 134.22 | -2.84 (-4.37, -1.31)c | -0.57 (-0.91, -0.22)b | |
| Not important | 3 | 191 | 72 (0.030) | 7.26 | 1.06 (-1.95, 4.06) | 0.16 (-0.37, 0.69) | |
| Interpersonal strategies | 0.190 | ||||||
| Important | 2 | 390 | 46 (0.180) | 1.84 | -0.59 (-2.50, 1.32) | -0.09 (-0.31, 0.13) | |
| Not important | 12 | 903 | 92 (< 0.001) | 140.01 | -2.30 (-4.01, -0.59)b | -0.48 (-0.86, -0.10)a | |
| Body directed strategies | 0.150 | ||||||
| Important | 5 | 694 | 67 (0.020) | 12.22 | -0.64 (-1.51, 0.22) | -0.19 (-0.43, 0.05) | |
| Not important | 9 | 599 | 91 (< 0.001) | 87.09 | -2.73 (-5.43, -0.02) | -0.50 (-1.01, 0.00) | |
| Homework assignment strategies | 0.640 | ||||||
| Important | 5 | 529 | 91 (< 0.001) | 45.80 | -2.60 (-5.42, 0.23) | -0.61 (-1.17, -0.04)a | |
| Not important | 9 | 764 | 91 (< 0.001) | 84.86 | -1.79 (-3.62, 0.04) | -0.31 (-0.72, 0.09) |
Five studies[26,27,30,33,40] with a total participant number of 369 analyzed the effect of CBT on stress symptoms. There were 184 patients in the intervention group and 185 in the control group. CBT-based interventions improved stress symptoms significantly with a pooled MD of -3.33 (95%CI: -4.23 to -2.44, P < 0.001) and a medium effect size of -0.62 (-0.83 to -0.40, P < 0.001). There was no significant heterogeneity between these studies (I2 = 22%, P = 0.280) (Table 2). Figure 2C presented the forest plot of the effect.
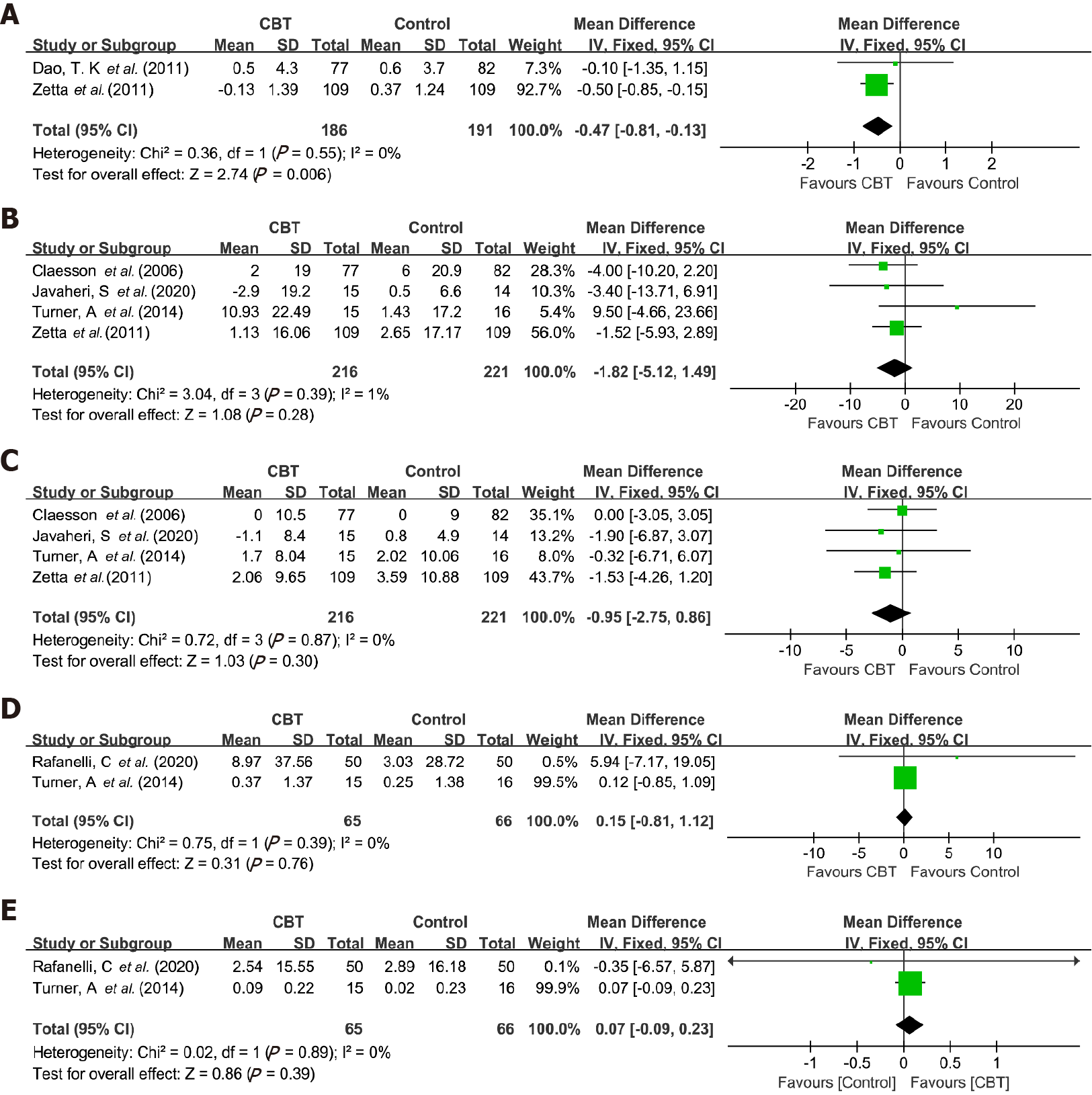
Effects on physiological factors: The effect of CBT-based intervention on BMI was analyzed in two studies[31,42] with 377 patients. There were 186 participants in the intervention group and 191 in the control group. Results showed that CBT-based intervention was more effective for reducing BMI levels than for the control conditions, with a mean reduction of BMI of -0.47 (95%CI: -0.81 to -0.13, P = 0.006), and a small effect size -0.23 (95%CI: -0.43 to -0.02, P = 0.030). There was no significant heterogeneity between these studies (I2 = 0%, P = 0.550) (Table 2). Figure 3A presented the forest plot of the effect.
Figure 3 Forest plots of the effects of cognitive behavioral therapy-based interventions. A: Body mass index; B: Systolic blood pressure; C: Diastolic blood pressure; D: Total cholesterol; E: High-density lipoprotein cholesterol. CBT: Cognitive behavioral therapy; CI: Confidence interval.
The effect of CBT-based intervention on blood pressure was analyzed in four studies[31,34,41,42]. There were 216 patients in the intervention group and 221 in the control group. The meta-analysis did not show a significant reduction either in systolic pressure (-1.82, 95%CI: -5.12 to 1.49, P = 0.280) or diastolic pressure (-0.95, 95%CI: -2.75 to 0.86, P = 0.300). Additionally, there was not significant heterogeneity for systolic blood pressure (I2 = 1%, P = 0.390) or diastolic blood pressure (I2 = 0%, P = 0.870) (Table 2). Figure 3B and C presented the forest plot of the effect.
Two studies[16,41] with 131 with 131 patients measured the effect on TC and HDL-C. There were 65 and 66 participants in the intervention and control group. We did not find a significant reduction in TC (0.15, 95%CI: -0.81 to 1.12, P = 0.760). Similarly, we did not find a significant improvement in HDL-C (0.07, 95%CI: -0.09 to 0.23, P = 0.390). There was not significant heterogeneity for TC (I2 = 0%, P = 0.390) or HDL-C (I2 = 0%, P = 0.890) (Table 2). Figure 3D and E showed the forest plot of the effect.
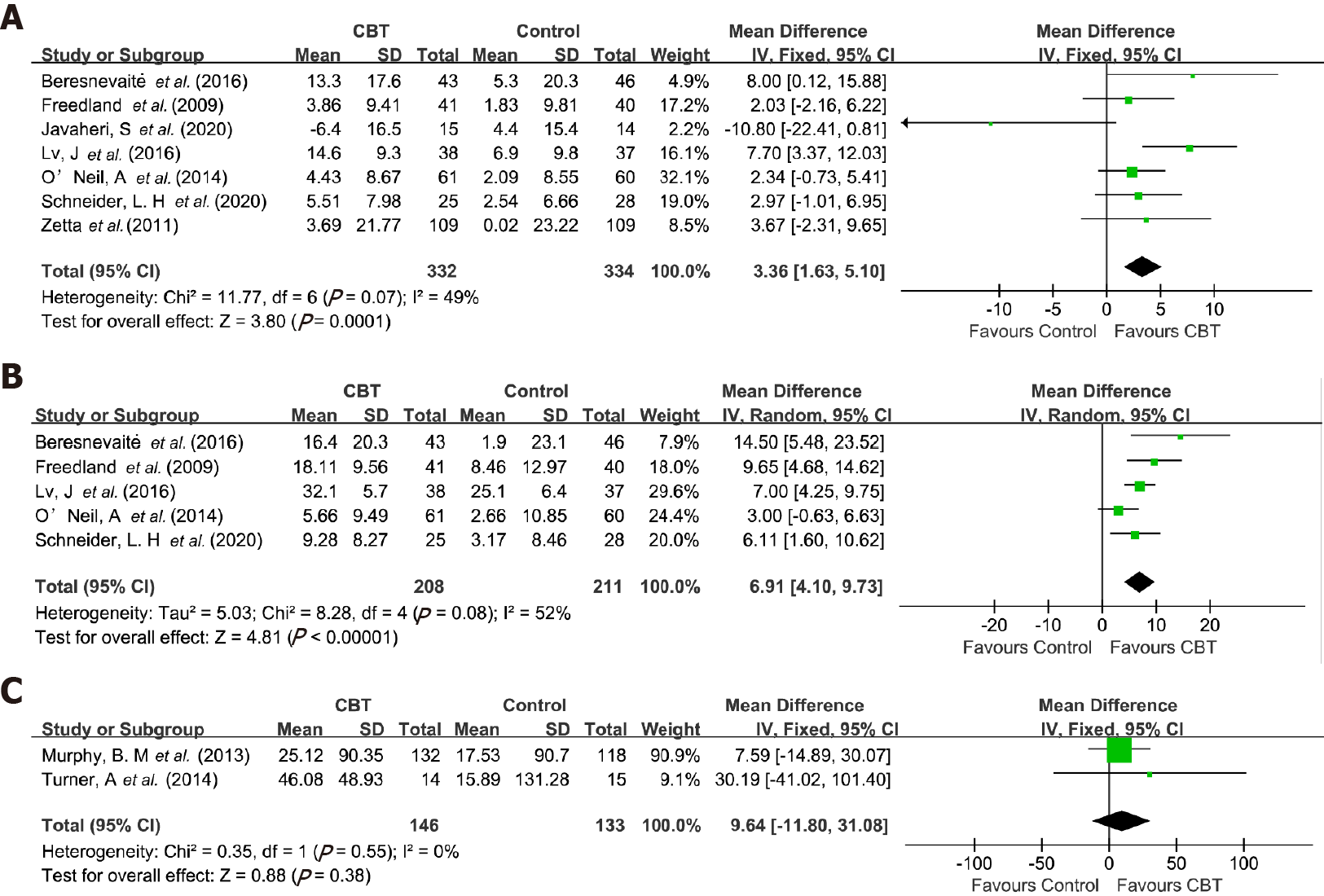
Effects on QOL and exercise endurance: The effect on physical function of the QOL was analyzed in seven studies[24,25,33,34,39,40,42] with 666 subjects. There were 332 and 334 patients in the intervention and control groups. Results showed that CBT-based interventions significantly improved physical function across seven studies with improved MD of 3.36 (95%CI: 1.63 to 5.10, P = 0.000) and a small effect size of 0.27 (0.12 to 0.43, P = 0.001). The heterogeneity between these studies was not significant (I2 = 49%, P = 0.070) (Table 2). Figure 4A showed the forest plot of the effect.
Figure 4 Forest plots of the effects of cognitive behavioral therapy-based interventions. A: Physical function; B: Mental function; C: 6-min walk distance. CBT: Cognitive behavioral therapy; CI: Confidence interval.
The effect on the mental function of the QOL was analyzed in five studies[24,25,33,39,40] with 419 patients. There were 208 patients in the intervention group and 211 in the control group. The pooled MD of improvement of mental function for CBT was 6.91 (95%CI: 4.10 to 9.73, P < 0.001) and a large effect size of 0.71 (0.41 to 1.00, P < 0.001). There was significant heterogeneity between these studies (I2 = 52%, P = 0.080) (Table 2). The forest plot of the effect was presented in Figure 4B.
Two studies[37,41] with 279 patients measured the change in exercise endurance. The number of intervention and control group participants was 146 and 133, respectively. We did not find a significant distance change between CBT-based interventions and control conditions (9.64, 95%CI: -11.80 to 31.08, P = 0.380). There was no significant heterogeneity between these studies (I2 = 0%, P = 0.550). The forest plot of the effect was presented in Figure 4C.
Risk of bias and quality assessment
The PEDro tool was used to evaluate the methodology quality of included studies, with one being high quality, accounting for 4.55%, and the remaining 21 being medium quality, accounting for 95.45%. Specifically, one study[39] scored 9, 11 studies[14,16,18,29,30,33,35,37,38,40,42] scored 7, four studies[25,27,31,32] scored 6, four studies[26,34,36,41] scored 5, and two studies[24,28] scored 4.
Publication bias
There was no T or P value of Egger analysis for BMI, TC, and HDL-C, because only two studies reported the results of CBT-based interventions on these variables. In Table 5, there was a minimal publication bias in the following outcome variables: depression symptoms (P = 0.467), anxiety symptoms (P = 0.196), systolic pressure (P = 0.516), diastolic pressure (P = 0.836), physical function (P = 0.829), and mental function (P = 0.135). However, the publication bias for stress symptoms (P = 0.021) was significant. We used the one-study-removed methods to evaluate the sensitivity, and we found that the overall results for all outcome variables were not changed when removing one study at a time. The funnel plots were in the Figure 5.
Table 5 Egger's regression analysis on publication bias.
| Variables | T | P value | 95%CI |
| Depression symptom | -0.75 | 0.467 | -2.60, 1.25 |
| Anxiety symptom | -1.37 | 0.196 | -7.36, 1.68 |
| Stress symptom | -4.42 | 0.021 | -9.65, -1.57 |
| BMI | - | - | - |
| Systolic pressure | 0.78 | 0.516 | -4.71, 6.80 |
| Diastolic pressure | -0.24 | 0.836 | -3.48, 3.12 |
| Total cholesterol | - | - | - |
| HDL | - | - | - |
| Physical function | -0.23 | 0.829 | -5.76, 4.83 |
| Mental function | 2.03 | 0.135 | -3.83, 17.40 |
| 6-min walk distance | - | - | - |
DISCUSSION
The results of our meta-analysis showed that CBT-based interventions were superior to the usual care controls. They reduced depression, anxiety, and stress symptoms, BMI levels, and improved physical and mental functioning in relation to the QOL. In addition, our subgroup analyzed several key identified components of CBT interventions that influenced their effect.
Post- to pre-treatment effects of CBT-based intervention
Effects on Psychological factors: Similar to previous studies[30,40], our study found that CBT-based intervention effectively reduced depression, anxiety, and stress symptoms in CHD patients compared with the control group. CBT-based interventions improve patients' knowledge about CHD through psychological education, and the corresponding cognitive and behavioral techniques contribute to the changes in non-adaptive beliefs of patients[43]. As for CHD patients with depression symptoms, their negative thinking mode can be altered through cognitive reconstruction[44]. For anxiety and stress emotions, the excitability of sympathetic nerves can be reduced through relaxation and behavioral techniques so that the mood can be improved[44].
We did subgroup analyses to found effective characteristics and components of CBT-based interventions in improving the symptoms of depression and anxiety in CHD patients. Firstly, CBT is more effective when it is provided as an individual rather than group treatment. The possible reason is that the individual treatment method is more targeted and more effective in treating the symptoms of depression and anxiety. Secondly, interventions that do not use a CHD-specific manual have a better effect on symptoms of depression and anxiety due possibly to the fact that the manual approach focuses more on the management of CHD rather than on negative emotions. This is consistent with the conclusions of research conducted by Yang et al[23] on diabetic patients. Thirdly, CBT is more efficient when it emphasizes psycho-education, behavioral and cognitive strategies as the core approaches, consistent with previous research conclusions, indicating CBT should highlight these strategies as the core[38,39].
Effects on physiological factors: Our meta-analysis found that CBT-based interventions have a significant effect on the reduction of BMI. The possible reason is associated with the improvement of health-related behaviors. Zetta et al[42] undertook research to analyze the effect of CBT in patients with angina. The intervention group patients reported increased knowledge awareness, fewer misconceptions, and an increase in self-reported exercise. Murphy et al[37] found a significantly reduced dietary fat intake among intervention group patients, indicating the favorable impact of the CBT and motivational interviewing program on patient nutritional habits. Thus, CHD patients' knowledge of the disease and their behavior habits may be improved through CBT-based interventions. They are more likely to maintain a good diet and moderate physical exercise to achieve weight loss goals.
Previous studies have found that CBT-based interventions can help to improve blood pressure and lipid profiles by reducing physiological stress caused by negative emotions, improving autonomic nervous system and endocrine system function[45]. However, we did not find CBT was effective in improving participants' blood pressure and lipid profiles. The possible reason is that only four studies reported on blood pressure and two studies on blood lipids. Both blood pressure and blood lipids have complex metabolic mechanisms, reflecting the need for a more significant number of studies to be conducted to assess the effect of CBT-based intervention on these factors accurately.
Effects on QOL and exercise endurance: Increasingly, QOL has become the focus of disease treatment and rehabilitation[46]. In this study, seven studies reported physical function, and five reported mental function. We found that CBT-based interventions can effectively improve patients' physical and mental function, consistent with previous studies[40]. It is possible that through CBT, the patient's negative mood is altered, improving their psychological state. At the same time, through techniques, such as behavioral activation, the exercise time of patients is increased, which is conducive to physical health.
The 6-Minute Walk Test is used to measure functional capacity[47]. As physical function improves, the 6-minute walking distance becomes longer. In contrast with our expectation, we found that the 6-min walk distance of CHD patients was not statistically improved through a CBT intervention. A possible reason for this finding is that only two studies reported this outcome variable. The improvement of a 6-minute walking distance is a long-term, complex process. The size of our sample was insufficient to draw conclusions about any changes in functional capacity.
Strengths and limitations of the study
The advantage of this paper is that it included 22 studies of moderate to high quality. In addition, unlike previous research, this paper also conducted subgroup analyses to explore specific characteristics of the CBT intervention, finding some critical components as described above. However, this paper also has some limitations. Due to the small number of articles included in the analysis, we must treat the results with some caution and conclude that more RCTs are needed to enhance the reliability of the evidence. Regarding other limitations, we only analyzed the results before and after the intervention and did not discuss the long-term follow-up results due to insufficient data. Therefore, there was a lack of long-term intervention effects of CBT-based interventions on CHD patients. Secondly, some studies were not able to use a double-blinded study design due to ethical reasons. Consequently, the quality of some of the evidence in this study may be not high. Thirdly, due to the limited number of studies reporting physiological factors, we need to be cautious in concluding the impact of CBT on these factors. Fourth, only articles written in English were included. Hence, it is possible that many eligible studies written in other languages were missed.
Implications
An increasing number of studies have applied CBT-based interventions to manage chronic pain[48], hypertension[49], diabetes[50], and cancer[51] and have found CBT interventions have been effective in improving health outcomes in these patients. Similarly, our meta-analysis found a positive impact of CBT-based interventions on psychological and physiological factors and QOL in patients with CHD. It is, therefore, reasonable to speculate that the use of CBT as a CHD rehabilitation program is effective. CBT can be incorporated into such programs in hospitals or communities. However, given there has been no standardized procedure for CBT-based interventions for CHD until now, it is advisable to infer that the regular supervision of experienced psychotherapists and psychologists is indispensable to guarantee the quality of CBT delivery.
CONCLUSION
This systematic review and meta-analysis findings suggest that CBT-based intervention is effective for CHD patients in reducing symptoms of depression, anxiety, and stress, BMI levels, and improving physical and mental functioning. In addition, the intervention may be more effective for depression and anxiety in CHD patients when it is delivered as an individual treatment method, when there is no CHD-specific manual, and psycho-education, behavioral, and cognitive strategies are applied as the main approaches.
ARTICLE HIGHLIGHTS
Research background
Coronary heart disease (CHD) is the most common coronary atherosclerotic heart disease, leading to adverse health outcomes for patients with CHD. Cognitive behavioral therapy (CBT) is a short-term psychotherapy, which has been increasingly recognized as an effective intervention approach to reduce psychosocial risk factors in CHD patients. CBT is to change an individual's non-adaptive thought patterns and beliefs, leading to positive behavioral changes. However, no comprehensive systematic review has been conducted to evaluate the efficacy of the CBT-based intervention on health outcomes in patients with CHD.
Research motivation
There is an increasing number of randomized control trials to investigate the efficacy of the CBT-based intervention in CHD patients. However, no comprehensive systematic review has been conducted, and there has been no meta-analysis of the effects of key components of CBT on health outcomes in patients with CHD.
Research objectives
This study aimed to synthesize results from previous randomized controlled trials (RCTs) using a meta-analysis method and explore the therapeutic effect of CBT-based intervention on health outcomes in CHD patients. The secondary aim was to analyze several key components of CBT interventions that explained the effects of CBT intervention.
Research methods
Relevant RCTs published in English were obtained by searching PubMed, Embase, Cochrane Central Register of Controlled Trials, Scopus, and Proquest, with the retrieval time from inception to August 2020. Review Manager 5.3 was used to conduct the meta-analysis. We used The Physiotherapy Evidence Database tool to assess the quality of included studies. Mean difference (MD) was used for continuous outcome variables, and standardized MD was used to measure the effect size. The random-effect model was used to estimate outcomes based on the heterogeneity testing. I2 was used for heterogeneity testing, and Egger regression was used to assess the publication bias.
Research results
A total of 22 RCTs were included in the systematic review and meta-analysis. The primary analysis revealed that CBT-based intervention significantly reduced depression, anxiety, stress symptoms, and body mass index (BMI) levels, and improved physical and mental functioning of the quality of life. Additionally, subgroup analysis found that CBT-based interventions were particularly effective in reducing symptoms of depression and anxiety in CHD patients when individual treatment form was used, and when psycho-education, behavioral and cognitive strategies were applied as the core treatment components.
Research conclusions
CBT-based interventions are effective in improving health outcomes in CHD patients, including reducing depression, anxiety, stress symptoms, BMI levels, and improving quality of life. Subgroup analysis further found CBT was more effective in reducing depression and anxiety symptoms in CHD patients when it is an individual treatment method, and when psycho-education, behavioral and cognitive strategies are emphasized as the core intervention strategies.
Research perspectives
Our research findings suggest that CBT is a promising approach in the health promotion of the population with CHD. However, the current practice in CBT-based interventions for CHD is not standardized, therefore, further research to standardize the CBT approach in clinical and community intervention programs in patients with CHD is needed.
Footnotes
Provenance and peer review: Invited article; Externally peer reviewed
Specialty type: Psychiatry
Country/Territory of origin: Australia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mizuguchi T, Oei SL S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
References
| 3. | Richards SH, Anderson L, Jenkinson CE, Whalley B, Rees K, Davies P, Bennett P, Liu Z, West R, Thompson DR, Taylor RS. Psychological interventions for coronary heart disease. Cochrane Database Syst Rev. 2017;4:CD002902. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 14. | Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, Czajkowski SM, DeBusk R, Hosking J, Jaffe A, Kaufmann PG, Mitchell P, Norman J, Powell LH, Raczynski JM, Schneiderman N; Enhancing Recovery in Coronary Heart Disease Patients Investigators (ENRICHD). Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289:3106-3116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1276] [Cited by in RCA: 1169] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 16. | Rafanelli C, Gostoli S, Buzzichelli S, Guidi J, Sirri L, Gallo P, Marzola E, Bergerone S, De Ferrari GM, Roncuzzi R, Di Pasquale G, Abbate-Daga G, Fava GA. Sequential Combination of Cognitive-Behavioral Treatment and Well-Being Therapy in Depressed Patients with Acute Coronary Syndromes: A Randomized Controlled Trial (TREATED-ACS Study). Psychother Psychosom. 2020;89:345-356. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 26. | Nehra DK, Sharma N, Nehra S, Kumar P. Efficacy of cognitive behavior therapy on perceived stress and health complaints in coronary heart disease patients. Indian J Pos Psychol. 2012;3:84. [Cited in This Article: ] |
| 27. | Nejati M, Sharifinia A, Maleki M, Bayazi MH. Comparison of the effectiveness of cognitive-behavioral group intervention for coronary heart disease and cognitive therapy in groups on type D personality and psychological distress on coronary heart patients- a randomized clinical trial. Curr Psychol. 2020;. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Barth J, Paul J, Härter M, Bengel J. Inpatient psychotherapeutic treatment for cardiac patients with depression in Germany - short term results. Psychosoc Med. 2005;2:Doc04. [PubMed] [Cited in This Article: ] |
| 37. | Murphy BM, Worcester MU, Higgins RO, Elliott PC, Le Grande MR, Mitchell F, Navaratnam H, Turner A, Grigg L, Tatoulis J, Goble AJ. Reduction in 2-year recurrent risk score and improved behavioral outcomes after participation in the "Beating Heart Problems" self-management program: results of a randomized controlled trial. J Cardiopulm Rehabil Prev. 2013;33:220-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | O'Neil A, Taylor B, Sanderson K, Cyril S, Chan B, Hawkes AL, Hare DL, Jelinek M, Venugopal K, Atherton JJ, Amerena J, Grigg L, Walters DL, Oldenburg B; MoodCare Investigator Team. Efficacy and feasibility of a tele-health intervention for acute coronary syndrome patients with depression: results of the "MoodCare" randomized controlled trial. Ann Behav Med. 2014;48:163-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |